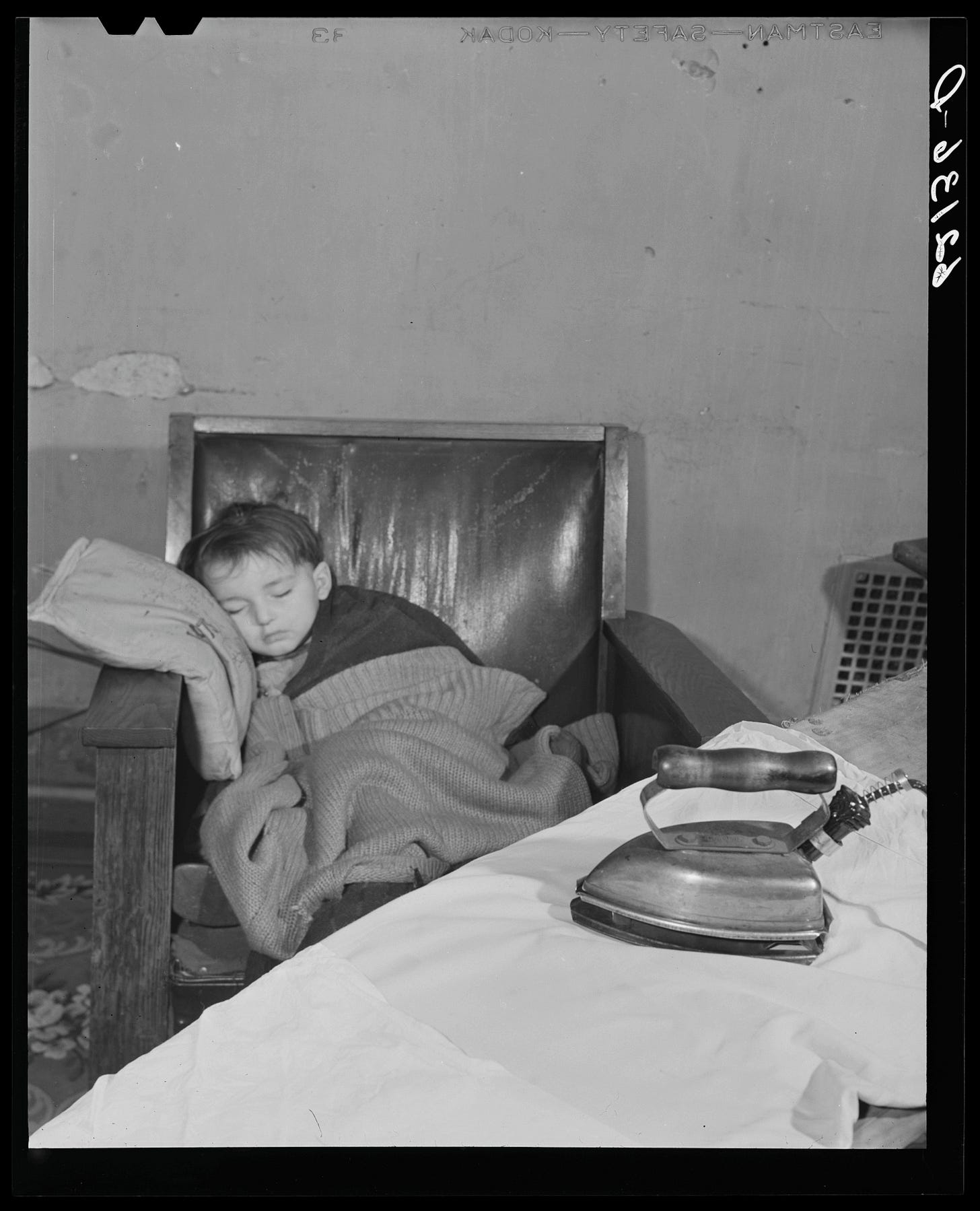
Innocent sleep,
Sleep that knits up the ravelled sleave of care,
The death of each day’s life, sore labour’s bath,
Balm of hurt minds, great Nature’s second course,
Chief nourisher in life’s feast
Macbeth, Act II, Scene Two
Americans have a rather strange relationship with sleep. At our universities, claims of “pulling an all-nighter” are worn as a badge of honor. At our hospitals, you will find physicians awake for nearly 30 hours continuously. Our Democratic and Republican leaders as well as our wealthiest individuals preen themselves on sleeping six hours or fewer.
The average American is not far behind, sleeping about 6.8 hours per night. The quality of this scant rest is rated as “fair” or “poor” by as many as one-third of Americans.
For optimal physical and mental functioning, nearly all experts recommend seven to nine hours of high-quality sleep each night. Indeed, when given a 16-hour opportunity to sleep, younger adults may opt to sleep about nine hours while older adults rest for close to 7.5 hours.
Based on conventional definitions, most Americans are sleep deprived:
Acute sleep deprivation is defined as sleeping fewer than seven hours for several consecutive days
Chronic sleep deprivation is when insufficient sleep persists for three months or longer
Acute sleep deprivation negatively affects alertness, attention, and vigilance, contributing to poorer performance in cognitive tasks compared to non-sleep deprived individuals. Acute sleep deprivation may also heighten anxiety and depression whilst impeding emotional intelligence and moral awareness, lowering subjective quality of life for oneself and others.
More severe health implications stem from chronic sleep deprivation, including increased risk of high blood pressure, type two diabetes, heart attacks, high cholesterol levels, depression, certain types of cancer, Alzheimer's disease, kidney disease, and immune dysfunction.
Most alarming, sleep deprivation may alter the perception of sleepiness and cognitive errors, limiting awareness of insufficient sleep. One may begin to believe they simply “need less sleep” compared to others and thereby lack motivation to rest more.
In this piece, we will explore the nature of sleep and mechanisms to improve its length and quality.
What is Sleep?
Measuring physiological changes in brain, muscle, heart, and eye activity during sleep identifies four major stages:
Rapid eye movement (REM)
Non-REM stage 1, called “NREM 1” or “N1”
NREM 2 (N2)
NREM 3 (N3), also known as “slow-wave sleep” or “deep sleep”
N1 is often only observed at the initiation of sleep. Sleep normally progresses from N2 to N3 to REM every 90 to 110 minutes with the portion of REM sleep in each cycle gradually increasing during the night.
REM Sleep
REM sleep plays a central role in learning and consolidating certain types of memory. Curiously, REM may help in remembering the factual components of an emotional experience (such as an argument with a spouse) while blunting the intensity of the memory, leading some to call this stage of sleep “overnight therapy.”
Although dreaming also occurs in NREM, dreams during REM are frequently more “elaborate, vivid, [and] hallucinogenic.” Muscles are largely paralyzed during REM to prevent dreams from being acted out. This paralysis is mostly absent in REM sleep disorders, frequently the harbinger of neurodegenerative conditions like Parkinson Disease and Lewy Body Dementia.
REM sleep usually occurs for the first time about 90 minutes after initiating sleep. “REM rebound” is observed in sleep-deprived individuals, in which REM sleep is entered almost immediately after falling asleep without first cycling through N1, N2, and N3.
Several psychoactive compounds decrease REM sleep, including alcohol, selective serotonin-reuptake inhibitors (SSRIs), lithium, trazodone and amphetamines. Only one major drug, reserpine, formerly used to treat adverse side effects of antipsychotics, is shown to increase REM sleep.
Deep sleep
Deep sleep is likely the most restorative stage of sleep. In addition to further consolidation of learning and memory, growth hormone is released, aiding in the repair of muscles and bones. The brain is also cleared of toxic metabolites and immune function is strengthened during slow-wave sleep.
Improving Sleep
Sleep hygiene refers to habitual behaviors that promote sleep quality and quantity. Although there is a burgeoning industry for sleep products, most mechanisms to optimize sleep are available at low to no cost.
There are several cornerstones to sleep hygiene:
The sleep environment should be kept dark, quiet, and cool
Physiological and psychological stimulation prior to bedtime should be limited
Bedtime and wake time should remain as static as possible
The sleep environment should be kept dark.
Exposure to excessive light before bedtime and during the night affects the onset of sleep, decreases the subjective quality of sleep, decreases total sleep time, and disrupts the progression of sleep stages by suppressing the amount of REM sleep and deep sleep.
These findings appear to depend on the wavelength of light present: blue light around 460 to 480 nm tends to be the most sensitive for shifting circadian rhythms. Higher color temperatures similar to daylight (about 7000 K) also provoke these effects.
There is some evidence for the efficacy of blue light-blocking glasses, but the data are mixed. Such glasses are likely best suited for individuals with insomnia and a condition called delayed sleep phase syndrome.
Other work suggests that bedtime exposure to red light and warmer color temperatures similar to candlelight (about 1800 K) may improve the quality of sleep.
Ultimately, complete darkness while sleeping is optimal. This environment can be achieved with use of “blackout” curtains on windows, although the use of an eye mask will likely be the most effective. An mask may also considerably improve subjective sleep quality. I recommend one with dedicated cups that encircle the eyes (see example) rather than a flat mask that functions as a shade.
The sleep environment should be kept quiet.
Loud noises naturally rouse one from sleep but findings suggest that intermittent noises above 35 dB have similar effects to light exposure by reducing deep sleep and total sleep time. For context, mild snoring is about 40-45 dB.
The use of a white noise machine as well as ear plugs can aid immensely in improving sleep quality by dampening the impact of both intermittent and loud noises.
The sleep environment should be kept cool.
Core temperature fluctuates naturally throughout the day, reaching its nadir near one’s habitual bedtime. Cooler temperatures can promote the initiation of sleep, reduce sleep latency, increase deep sleep, and boost overall sleep time.
The ideal bedroom temperature is about 60 to 68°F (16 to 20°C). Some mattress pads have embedded temperature regulation technology that lower core temperature. Although internal research by the most popular mattress pad company, Eight Sleep, suggest their cover improves total sleep time, REM sleep, and deep sleep, these findings have not been independently verified. As their mattress pads start at $1800 and require a monthly subscription to utilize all features, it is prudent to wait until additional research is conducted until you “invest in your rest” to this extent.
Limiting stimulation
Optimizing one’s sleep environment requires reduction of psychological and physiological arousal prior to initiating sleep.
Moderating Internet use functions in concert with restricting blue light exposure. Using electronic devices before bed can markedly lower the subjective quality and duration of sleep. They should ideally be avoided for an hour or more before bed. Notifications sent to a wearable device should likewise be silenced during this time.
Consumption of caffeine, the world’s most widely used stimulant, should be abstained for several hours before bed. A recent systematic review concluded that a cup of coffee (about 100mg of caffeine) should be avoided about 9 hours before bedtime to prevent significant decreases in total sleep time. Other work found that just 200mg of caffeine (about two cups of coffee) sixteen hours before the onset of sleep led to a significant decrease in total sleep time and efficiency.
Avoiding caffeine for even a day can substantially improve sleep quality. No one in their right mind will do that, of course, so we should instead focus our efforts on more judicious use of caffeine during the day to limits its ill effects on sleep.
Other means to reduce stimulation include the association of certain aromas with sleep (such as lavender), practicing deep breathing, or listening to relaxing music.
Exercise and sleep
Broad research trends point towards the role of exercise in sleep efficiency, quality, and duration while reducing symptoms of sleep disorders.
Among young adults, moderate-intensity exercise (Zone 2 training) performed 6 hours before bedtime and high-intensity exercise (Zone 5 training) 3 to 4 hours before bedtime significantly increased slow-wave sleep.
Some work suggests that moderate-intensity exercises ending 90 minutes before bedtime does not negatively affect any major sleep parameter. Vigorous exercise ending within 30 minutes to 4 hours of bedtime, meanwhile may decrease REM sleep. Similarly negative effects on sleep latency, total sleep time, and sleep efficiency were observed when high-intensity exercise ended within a hour of bedtime.
Among middle-age and older adults with poor sleep quality, moderate exercise may bolster subjective sleep quality as well as total sleep time.
For adults of all ages, moderate-intensity exercise may ultimately have a more pronounced and beneficial effect on sleep quality compared to vigorous exercise. Both types of exercise are nonetheless important components of a long, enjoyable life.
In the interest of caution, moderate-intensity exercise should be completed within about 90-120 minutes of bedtime and high-intensity exercise should be avoided within four hours of bedtime.
Habitual timing of sleep
Although deplored as an anachronism of childhood, maintaining regular bedtimes and wake-times are vital to receiving consistently high quality sleep.
Some work suggests that sleep regularity is a stronger predictor of all-cause mortality than sleep duration. Irregularity in sleep is a more direct proxy for circadian disruption, itself linked to adverse effects on physiology.
In late 2023, the National Sleep Foundation released an updated expert statement on sleep consistency, stating broadly:
“Regular [sleep] schedules were associated with improved outcomes across multiple dimensions of health and performance, including alertness, health and safety behaviors, cardiovascular health, metabolic health (including fasting glucose, hemoglobin A1C, and metabolic syndrome), inflammation, mental health (including depression, mood, and suicidal ideation), academic performance, cognitive performance, sleep duration, and sleep quality.”
Such regularity can be especially difficult among younger adults, who are prone to “social jetlag” in which societal obligations during the week dictate earlier wake times compared to biological preferences. Frequent social jetlag longer than two hours is associated with higher levels of cortisol, increased resting heart rate, and depression.
On weekends— or days in which there are no social obligations—individuals tend to sleep at times more aligned with their biological clocks. These sleep patterns often reveal our chronotypes, or circadian preferences. Classically, populations are divided into morning types or “larks” and evening/night types or “owls,” although 60% of individuals have circadian preferences in between these two extremes.
As anticipated, evening types experience more social jetlag during a standard workweek, contributing to shorter sleep duration. Independent of sleep duration, evening types are at elevated risk of high blood pressure, sleep apnea, type two diabetes, and obesity, contributing to higher mortality rates compared to morning types.
Chronotypes tend to gradually shift earlier starting in early adulthood and may move forward about 11 minutes over a seven-year period.
Although we are bound by our biology and unable to drastically modify our circadian preferences, we can still work to normalize our sleep schedules by going to bed and waking up within the same one- to two-hour window each day.
Thus, if one generally goes to bed at 10:30pm and wakes up around 6:00am, an optimal delayed shift would require a bedtime of 12:30am at the latest with plans to wake up at 8:00am.
At the same time, if sleep was insufficient (i.e., fewer than seven hours) during working days, obtaining an extra 1-2 hours of sleep on non-work days may be beneficial even if waking time falls outside of the stipulated window.
Sleep debt is the amount of sleep lost when sleeping fewer than seven hours. It may also be conceptualized as the gap between one’s optimal amount of sleep and habitual amount of sleep.
If sleep debt during a typical workweek amounts to five hours (i.e., sleeping six hours each night for five nights), it might be difficult to sleep for a period of 9 to 10 hours on each weekend night to make up for this sleep debt. To be sure, only a quarter of individuals who accumulate sleep debt greater than 90 minutes during the workweek may be able to obtain enough rest on weekends to compensate for this shortfall.
Nonetheless, some work suggests that extended sleep on weekends may mitigate the enhanced risk of mortality that stems from insufficient sleep during the week, defined as five hours or fewer of sleep on average.
Wearables
Sleep efficiency refers to the total sleep time relative to the overall time allocated to sleep. A sleep efficiency above 85% is generally regarded as healthy; at that level, one would sleep for 6.8 hours if given an eight-hour sleeping opportunity.
Sleep latency refers to the duration required to transition to sleep. A healthy sleep latency is about 10 to 20 minutes. Sleep deprivation can reduce sleep latency to fewer than 10 minutes. Sleep latency less than five minutes is conventionally considered diagnostic for excessive sleepiness and may suggest an underlying condition such as narcolepsy or idiopathic hypersomnia, especially when REM rebound is also observed.
Insomnia is generally considered present when sleep efficiency consistently dips below 85%. Sleep-onset insomnia is difficulty falling asleep whereas middle and late insomnia refer to difficulty falling back asleep in the middle of the night or early morning, respectively. Sleep-onset insomnia lengthens sleep latency (> 20 minutes) and contributes to lower sleep efficiency.
Even without knowing your average sleep efficiency and sleep latency, a good rule of thumb is adding an extra half-hour to your target amount of sleep. If you aim to sleep for seven hours, seven and a half hours would then be spent in bed.
Most wearable devices can provide a broad sense of both sleep efficiency and sleep latency. Both sleep efficiency and sleep latency are often overestimated by these devices, however, and their ability to classify NREM and REM sleep stages remains poor when compared to the gold standard of measuring electrical brainwaves through EEG. Their data should be considered with a grain of salt.
Supplements
The most popular sleep supplement is almost certainly melatonin, a hormone released naturally by the brain to facilitate the onset of the sleep, likely through its effect on core body temperature. The pineal gland in the brain produces 0.1 to 0.8 mg of melatonin per day.
Melatonin levels rise slowly around one's habitual bedtime and peak during the middle of the night before maintaining a trough near waking. Melatonin is notably sufficient but not necessary for sleep: daytime levels of melatonin are essentially non-detectable but napping remains possible.
Supplemental melatonin significantly reduces sleep latency, increases sleep efficiency, and lengthens total sleep time in subjects with and without sleep disorders. Tolerance to melatonin is rarely documented within the literature although anecdotally some individuals who habitually use melatonin find they must escalate dosage to obtain the same effect of drowsiness.
Given the extensive interaction between melatonin and sex hormones, there is some concern that long-term use of melatonin may interfere with pubertal development. There is insufficient evidence at present to suggest regular use of melatonin does or does not affect puberty. One study in adults showed nightly use of 1 mg melatonin over one year led to significant increases in prolactin but left other hormones unaffected. High levels of prolactin may impede reproduction, but the literature does not conclusively show that melatonin carries this clinical effect.
Like other supplements, melatonin is not regulated by any government agency, and there may be a discrepancy between the dosage on a label and the actual content of a product.
Magnesium and glycine are increasingly popular sleep supplements, promoted largely by podcast hosts. Results regarding magnesium and sleep are mixed without a clear consensus on its efficacy. Improved sleep quality and decreased sleep latency have been observed with short-term use of glycine though long-term use data is very limited.
In certain circles, ashwaganda is regarded as a cure-all with applications as an anti-depressant, anti-inflammatory, and antioxidant among others. Use of ashwaganda for greater than eight weeks may improve sleep quality among individuals with sleep disorders but safety data regarding long-term use is limited.
Aperçus on sleeping too little and too much
Perhaps the only useful application of insufficient sleep is in the treatment of depression. Therapeutic sleep deprivation (SDT) was first described in 1971. A single night of total sleep deprivation has been shown to improve depressive symptoms in about 40-60% of patients, effects which vanish for most after a subsequent full night of sleep.
One meta-analysis showed sleep deprivation for fewer than seven days or more than fourteen days worsened depression while sleep deprivation for seven to fourteen days had a robust anti-depressive effect.
Some work also suggests a potential benefit of sleep deprivation in alleviating symptoms from Parkinson disease. Improvements in motor function were observed in a Parkinsonian animal model but were not replicable in human subjects. Conversely, there is a documented sleep benefit that occurs in Parkinson disease in which symptoms improve for about 80 minutes after waking, allowing some patients to delay taking their first dose of medication.
There is a well-documented association between chronic sleep deprivation and higher rates of mortality. Curiously, excessive sleep also shows this relationship, leading to a “U”-shaped curve between mortality and sleep duration in the literature. In other words, individuals who sleep either the least or the most have higher rates of mortality compared to those who sleep about 7 to 8 hours per night.

Does this mean that we should be wary about sleeping more than nine hours per night? Probably not for at least two key reasons:
Sleep duration in this work is usually measured subjectively through questionnaires— participants are simply asked to recall how much they slept last night. Compared to objective measurements, individuals tend to overestimate how much sleep they received, suggesting these data may have significant recall bias.
Important risk factors for mortality such as diabetes, coronary heart disease, and obesity may be more common in individuals who self-report sleeping longer (defined in this review as >9.5 hours). More, long sleepers are more likely to be older than 65 years and these data “may represent an end-of-life process with progressive fatigue and inactivity.”
Taken together, the causal chain is more likely to be:
Significant risk factors for mortality → longer sleep
And not,
Longer sleep → heightened risk factors for mortality (as some observers tend to report)
In other words, these underlying health conditions are an interaction variable that simultaneously increases mortality risk and sleep duration. Without careful parsing, one may conclude spuriously there is a positive relationship between sleep duration and mortality.
Although this explanation makes good sense to me, the mechanisms driving the correlation between extended sleep and mortality has not been robustly elucidated in the literature beyond an elegant article by Léger et al. (2014).
Sleep like the veranda of a country house
spreads before you a forest and shadows
and the interior of memories.
Sleep is the mind free of constraint,
the proud capital of poetry and plays,
sleep is a thought not yet embodied,
fed meagerly by jealous waking.
The Majesty of Sleep, Adam Zagajewski








Sleeep, as discussed in this holistic treatise, is perhaps the most sought ‘commodity’ by many, especially the Quality sleep-the deep kind of “sleeping like a baby”-what Does a baby dream?-and presented are some appreciated roads to achieve it. Good reading